This article is my journey through nightly traumatic pain events. At the beginning of this article I do not know exactly what is going on and at the end I have a clear understanding of what is happening and how I treat it, along with a sleep disorder clinic’s concurrence.
About every other day I wake up to what feels like I am about to have an aneurism. No, I haven’t had one, but I fear one may develop and the pain can be severe. I believe it is related to a sleep disorder called Cyclic Variation of Heart Rate, CVHR and Obstructive Sleep Apnea, OSA. I also now suspect a hypnic headache in the mix, something I didn’t find out about for another nine months.
https://www.ahajournals.org/doi/10.1161/CIRCEP.110.958009
Episodes of OSA are accompanied by a characteristic heart rate pattern, known as cyclic variation of heart rate (CVHR), which consists of bradycardia during apnea followed by abrupt tachycardia on its cessation.
What is not described in that disorder is what comes right after its symptoms, namely blood rushing to my brain under pressure that I believe could lead to an aneurism. Its painful and I don’t yet have it under control. The tachycardia is sometimes a slightly faster heart beat than normal but more powerful than normal as well.
Cyclic Variation of Heart Rate Symptoms
I have sleep apnea, that is where you wake up realizing you are not breathing. Sometimes you are gasping, and its a natural response, but in my case, at the moment, I simply wake up and decide to start breathing. There is a controlled calm response to it. Generally this happens to older overweight individuals where the weight of the body causes the airway to close off during sleep. I also have a slow heart rate, Bradycardia, at night when I sleep, somewhere in the high 40bpm to mid 50bpm for some length of time at night resting. Cyclic Variation of Heart Rate, CVHR, is described as occurring during Bradycardia and upon waking during REM sleep due to an apnea event. Upon the initial respiration after this event, i.e. upon taking the first breath, an arrhythmia is triggered, a fast heart beat.
The trigger for me is immediate. It took me a bit to see the relationship because I’m usually groggy when I wake, but lately I wake very calmly and I know what is going on with my body.
In other words, I’m sleeping and I wake from a vivid dream because I realize I’m not breathing. I should add, I have had vivid dreams for seven months, every single night, many months before this started. Knowing you have a vivid dream generally means you woke up during that dream and stayed awake long enough to remember it. In my case, this is not dramatic. I’m not gasping for air. I simply decide to start breathing. I’m awake, I realize what I’m doing and I take a nice breath. For a split second it feels refreshing, and then my heart beats really fast. This is an arrhythmia.
Beyond Cyclic Variation of Heart Rate
For me, the heart rate is not just fast, its hard, though it can vary sometimes and simply be tachycardia, a fast heart rate. There are four or five hard heart beats that send blood rushing to my head. I feel veins in my neck at the base of my skull throb and I can hear the blood rush, whoosh, whoosh, whoosh, into my brain.
This generally does not hurt at first. It sometimes can move around to my right temple where veins there do the same thing. This feels like migraine level pain shooting through with each heart beat. Since I’m very tired and groggy at the time and the heart beat subsides and the pain goes away, I simply fall asleep again. Total duration of attack is about 10 seconds. However it repeats each time I awake from a dream until I finally get up in the morning. If it goes on long enough it can continue on in to the waking period. By that I mean throbbing events with pain, not simply a general headache.
The events either involve blood pumping through the base of my skull, throbbing and then moving to the right temple or the throbbing at the base of the skull is skipped completely and I feel it in the right temple only. Usually prolonged base of the skull events lead into right temple. A night with just right temple events is much worse. These events almost always continue until I fully wake for the next day. By continue I mean the events happen again every time I wake up. I am not in pain as I sleep or past the ten seconds or so of the event. I do not believe Cyclic Variation of Heart Rate is the only thing going on.
Additionally, if it continues too long my brain will feel foggy during the day. I am not cognitively impaired or slowed. That is not what I mean. Waves of numbness flow from one side to the other, almost like electricity, but slower.
How I Have Learned to Cope
This has gone on regularly for about six weeks. I have experienced this in the past but usually on a frequency of once or twice every six months and never back to back. At present it happens about every other to every third night. I have tried sleeping with my head elevated. This is to try to reduce the number of apnea events. Remember, CVHR requires a slow heart rate and an apnea event during REM sleep, the period where you dream. So if I stop the apneas, or prevent them from happening during REM sleep, then I stop the disorder, and if I stop the disorder, I stop the follow-on effects that I am experiencing. [In the end, this failed.]
Changing Medications
I tried changing my medications, stopping some, changing when I take them, and so far have not found a reason this has started. I also take Levothyroxine for Hypothyroidism. It is possible that not taking that helps. But I have taken it and not had the event happen as well. I tried to change when I took this medication to nighttime to see if it would elevate my heart rate to help avoid the events that way. This had no impact. As of Feb 11, 2022 I have found no benefit to medication change.
Change Sleep Position
Sleeping on a wedge in bed did not help. I end up sliding down or compressing the wedge because it is too soft. This can be solved with a wedge made of harder foam and possibly something beneath my butt to stop sliding. I have read that raising the head, elevating it more than seven degrees can help prevent sleep apneas.
To change my position and address compressing the pillow, I have changed to sleeping in a recliner. I have to make sure I don’t recline too far and end up flat again but it does seem to help. However, it is not 100%. I still have “events” sleeping in the recliner. In the end, I chose to abandon this and return to bed as it did not stop the events and was horrible sleep. My pulmonologist said I will have sleep apneas, that the goal is to get them below 5 per hour and I am down to 2. He feels it is under control from that perspective of whatever is going on here, Cyclic Variation of Heart Rate or not.
Doctor Recommended Medication
In the last couple of days I have started taking 1.5mg of Melatonin after a doctor recommendation. I also feel Ibuprofen is beneficial but have yet to take either long enough to determine if they are a cure. I have taken Ibuprofen on nights when I did not have events.
Let me add, I took 5mg of Melatonin the first night it was prescribed and had horrible events. Somewhere close to ten “events” in the matter of an hour or two. It was not a solution, actually if this was the prescription I would refuse it. But I also read Melatonin dosage can be tricky. I didn’t know because the doctor didn’t tell me. So I reduced to 1mg to 2mg, also checked with my doctor and he confirmed, and the last two nights have been good, sleeping on a recliner with a CPAP. [In the end this proved not to help.]
Expect Updates
These events first began back in at least November of 2021, every other night approximately. This blog was start on January 22, 2022. I have had two decent nights in a row and will update with what solves this for me, if anything. I do have a referral to a neurologist and another for a pulmonologist. I’ll have them wrestle for who fixes me first. [spoiler, they suck at wrestling]
- Jan 23, 2022 – I had 2 mild events at 6am as I woke. Oddly, not the first breath after waking but when I took deeper breaths. This has happened before when there are multiple attacks during a night that tire me and create the conditions for it to carry in to the waking period. Definitely right after waking from a dream, so REM sleep. My position in the recliner was too flat. I’ll raise the Melatonin to 2mg and try better to stay elevated.
- Jan 31, 2022 – I’ve raised it to 2.5mg before bed with 1 Ibuprofen. If I wake at night after a couple of hours I’ll take another 1.5mg. No events in the last two days. One minor event three days ago. I still sleep in a recliner. Events generally happen every other to every third day, so I’m still not successful until I can eliminate the events, certainly beyond 3 days, preferably a minimum of a week and of course the goal is forever.
- Feb 5, 2022 – So far I haven’t gone beyond 4 days without an event. I’ve raised Melatonin to 3mg to start with an added dose of 2mg if I wake up at least four hours later. I know Melatonin isn’t the end solution because 5mg before bed still had me with major events all through my first night using it. This is where I will stay for now.
Still sleeping on a recliner to elevate my head to avoid apneas. On the days I workout I have an easy time sleeping and no events that I can recall. That usually has me with a higher heart rate at the beginning of the night. - Feb 11, 2022 – So far, still haven’t gone past a couple of days without events. But I believe 400mg of Ibuprofen alleviates the throbbing and pain. It doesn’t throb and therefore no pain even as I continue to have an arrhythmia. The fast heart rate after waking and breathing is still happening but without corresponding overload to the arteries in my head. I’ve read about temporal arteritis but don’t yet see enough symptoms, not that I want to wait. Ibuprofen being an anti-inflammatory may help. So far, only two nights in a row with success, but last night I expected issues and had none. I worked out today and do not expect issues due to an elevated heart rate as a result.
A couple of days ago I had multiple events rather early in the evening, 10:58pm to start. These were right temple throbbing events, not base of the skull. These lasted a couple of hours. I could feel it coming on before I went to bed. I knew it was going to be a bad night. Sort of an electricity in my head. Then my second dose of I believe Ibuprofen and Melatonin seemed to stop it. I had no further events after about 3am on into the morning. This was unusual. As morning went on, each time I awoke I felt more confident the events had stopped for the night. - Feb 21, 2022 – Tonight, despite taking 400mg of Ibuprofen right before going to sleep I ended up having multiple events all throughout the night starting 3 hours after going to sleep. I took another pill after 6 hours and the events continued unabated. I then took a migraine pill my doctor gave me and that had no effect as well. Sleeping in a recliner is worthless for me. Ibuprofen isn’t helping despite a fairly good week. If it were that, it would have worked last night too. What I still think helps is a solid workout that day and evening that keeps my heart elevated right up until bedtime. But that could all be crap as well. I’m working out more and those nights that I do I have yet to have an event.
I’m moving back to bed and no more Ibuprofen as a deterrent. Not supposed to take it long term anyway. I still haven’t gotten an appointment for a neurologist yet. That is my only hope. - Feb 26, 2022 – My doctor prescribed a sleeping pill, Eszopiclone 3mg. Sure, I sleep, for about 4 hours and then there is the chance the events start happening again. First two nights were fine, but on the third they happened again. After about two events I took 400mg of Ibuprofen and they stopped, but then I was light sleeping till I woke. Ibuprofen will stop the events after a bit but is not a guarantee to prevent and if they don’t you can’t take more until 6 hours pass. Ibuprofen also isn’t supposed to be used long term, though my dose is at most 600mg a day. I keep it by the bed. I won’t be able to prevent at least one attack a night, but I think I can prevent the rest. Again, its not about headache pain, its about the pressure in the arteries and Ibuprofen does appear to stop that.
- I’ve been taking Eszopiclone 3mg and 200mg of Ibuprofen before bed. It worked great for two days. This morning I had a couple of attacks, minor, and took another Ibuprofen to ward off further. That didn’t help. It seems to help sometimes, and maybe things are better as a result. Some nights are perfect. But it is not 100%. I’m switching to just the sleeping pill, making sure I’m super tired before I go to bed. Ill keep 400mg of Ibuprofen to ward off attacks after the first happens or maybe take those if I wake in the night. I see the pulmonologist tomorrow, hopefully he knows about Cyclic Variation of Heart Rate and then whatever this is that is following it in my case.
- Mar 3, 2022 – I went to Pulmonologist today. He said my CPAP reading looks good. He can’t help me. Said I need a neurologist or rheumatologist. He had not heard of this kind of presentation of symptoms before. Mentioned Giant Cell Arteritis. My symptoms only partially fit, though it is the major symptom that fits.
- Mar 4, 2022 – I went to my rheumatologist today. Told him about the symptoms. He said it sounds like a migraine. I asked is it nerve pain or blood flowing through the arteries and he said its blood flowing through the arteries that I’m feeling. That doesn’t sound like a headache to me, but I’m not a doctor. He said its the artery close to the skin, because I can feel it, and that its unlikely for me to die in the middle of it. That aneurisms that kill are deeper in the brain and you don’t feel the pressure like I’m describing. He doesn’t think I can get arteritis on the drugs I’m on, but I did forget to tell him I’ve had these symptoms for 6 years, just not every other day like right now. However, I’m getting lab tests done to look for markers of arteritis. Also said to push for neurologist outside of my current system since its so jammed.
- Mar 7, 2022 – I’ve had four good nights after taking Tamsulosin. I have a kidney stone that may be on the move a bit and I want to make sure to do what I can to keep things going and decided to start using it again. Whether its helped or these are just four random good nights I do not know. I am also still taking the sleeping pill. I woke at 4am and was up a bit. No reason last night was good other than possibly this medication change, and of course still no reason for it to be happening anyway.
- Mar 15, 2022 – Ten good nights, but last night I had throbbing in the base of the skull again. After two attacks I took 400mg of Ibuprofen. I took my blood pressure and it was 107/72, so high blood pressure is not the cause. I’ll continue surveying events at night when I can to be sure. My blood pressure during the day was 135/80. I had one more attack and then they stopped and I slept well for a couple more hours even with some waking afterwards. It takes a bit for Ibuprofen to kick in and bring me out of whatever zone it is that causes these things, IMO, assuming it isn’t just luck. I am not a doctor, these are my observations. Neurology appointment scheduled in two days.
- Mar 28, 2022 – Since my last post I have had two nights of minor attacks and one with fairly annoying right temple attacks. I’ve also seen a neurologist and had an MRI and EEG. Best I can tell so far is I think its a cardiologist I should see, but there could be cross-over. Results in a week. The other thing is, in that time, I’ve been working out and walking daily other than before the nights of attacks. I believe the exercise being anti-inflammatory is related and that is my current plan to stop these things. I walk an hour or I walk down to the gym and work out and walk back, totaling an hour workout. Nothing else helps and to the best of my memory I have not had attacks after workouts.
- Apr 7, 2022 – I’ve had an MRI and EEG at this point and the results showed no damage. I’ve had two more attacks, one where they just kept coming, as if I was riding a wave at the edge of coming awake. I woke up, took 400mg of Ibuprofen and stayed awake until I knew it had time. No repeat, however I did have another Ocular Migraine the next day. This is where I look at a lamppost or any object and I can see a duplicate a couple of inches higher, ghosted.
The neurologist is going to try migraine medication to see if it can shift my brain into a different mode to avoid these events, at least the throbbing pain part, which is inline with migraine descriptions as far as they are concerned. The heart part, which I describe as Cyclic Variation of Heart Rate, he will leave to a cardiologist, and so that is my next referral request. - Apr 25, 2022 – Neurology dosage hasn’t really helped. I had three attacks while on it. Told them, they didn’t seem to care. Just noted it in my chart and said see you in 6 weeks. WTF. My doctor raised the dosage of the migraine meds by half a pill. It seems to be helping. Whether it stops them or I just sleep through them with less pain I don’t know. Dates are blending together. I think I still had one on this dose when I woke up one morning, along with a headache. Other than that, clear for 6 days.
- May 13, 2022 – I’ve been to a cardiologist. He recognizes the Cyclic Variation of Heart Rate symptoms but did not know anything about the pain I experience during it. Before bed I take 35mg of Amitriptyline and Eszopiclone (a sleeping pill). This does not stop the attacks. It does seem to reduce them or reduce their pain. I wake up fewer times and thus have fewer opportunities for an attack to occur when I’m in whatever state that causes this. High heart rate at bed time does not 100% stop the attacks, but does severely reduce them.
The cardiologist mentioned a pace maker for the diaphragm, but I don’t think that will end up being appropriate as that is for people otherwise on ventilators. I suspect a heart pace maker to keep me above Bradycardia is more likely. But that again is a question as recently I believe I’ve had attacks at higher heart rates.
Neurologist and cardiologist appointments coming again soon. - June 1, 2022 – No progress on the medical front. What I have found is if I work out such that my heart rate is 91bpm at 10pm when I go to sleep I can avoid the issue. The assumption is it takes long enough over the night to cool down that I avoid Bradycardia during a critical period of sleep. This has succeeded for about 3 weeks.
- July 26, 2022 – Cardiologist reports the echo of my heart was perfect. If I had central sleep apnea, simply not breathing for no apparent reason while sleeping, they would give me a pacemaker for my diaphragm, but my sleep study does not show it. I don’t really want one, but if this isn’t just pain I also don’t want damage to add up over time. As of now they say they cannot help. I’ve fallen in some crack between specialists and I was on my own again.
I am now attempting to work with University of Florida sleep specialists. They also have not heard of the follow on throbbing pain that I describe. We will do a new sleep study to confirm lack of central sleep apnea and likely other specific points of interest. After that, possibly some test of the electrical system of my heart.
I am taking 75mg of Amitriptyline along with weight lifting as hard as I can such that my heart rate stays above Bradycardia to avoid Cyclic Variation of Heart Rate. I work out about an hour and forty-five minutes a day, with some portion in the evening in the hope that my heart rate is still in the 90bpm area at 10pm. Weekends are the danger zone, gym closes at 3pm. It is this work out that primarily keeps the attacks at bay, though I am hopeful the new dose of medication will help on off days. I also still take Eszopiclone 3mg to help with sleep.
I will add that I again had one night where I had three attacks back to back, like I was riding on the edge of sleep and as each attack ended my next breath would trigger a new one. - July 28, 2022 – 75mg of Amitriptyline is not enough, going to new dose of 85mg. I worked out on my easier workouts of the series and my heart rate wasn’t high enough. I had multiple events that night.
- August 8, 2022 – 100mg of Amitriptyline is not enough. I’ve asked to come off of it and be given a new medication, but the neurologist just said I have an appointment in 9 days so I can talk in person about it then. My feeling is they don’t like doing things without an appointment because that is how they get paid. Not happy. I’ll come down off of Amitriptyline on my own.
Heavy walking on a hot day does help as it appears to keep the heart rate high at night. Normal walking does not help as I have already tried. I had two full says in Disney parks and did not have issues while there, likely due to activity.
I just ran across an article that I hope will help. I had read about hypnic headaches before, but the article described too many things that sounded different than what I was experiencing. I now hypothesize that I have a silent hypnic headache that when I wake due to an arrhythmia as a result of Cyclic Variation of Heart Rate, CVHR, causes my heart beat to race pushing blood through constricted veins causing elevated pain with each pulse. REM sleep is also a factor, as I believe waking during dreams is typical.
One article states that I could have obstructive sleep apnea AND hypnic headache.
“Other secondary causes include temporal arteritis, obstructive sleep apnea (OSA), hypoglycemia, psychiatric disorders, and chronic pain disorders.34-40 A diagnosis of OSA does not eliminate the possibility of a concurrent HH diagnosis.41”
I believe that while I happen to wake early in the process, as opposed to as the pain hits, or at least I often wake first, that I do have a type of hypnic headache. It may be that in other research they didn’t encounter the same precursors. So, to go along with my hypothesis, I will begin taking 100mg caffeine pills before bed, along with a sleeping pill and some Melatonin. Yes, uppers and downers mixed. Note, just prior to onset of these headaches last October, I stopped drinking caffeinated sodas. I don’t know of anything right now that would give me caffeine. Which could explain the timing and possible intermittence of symptoms all this time, between working out and how hard each day might be and whether or not I happened to have a soda containing caffeine, which has been rare this past year.
Some other relevant research links:
https://www.sciencedirect.com/topics/medicine-and-dentistry/paroxysmal-hemicrania
https://americanmigrainefoundation.org/resource-library/parosyxmal-hemicrania/
https://www.sleepfoundation.org/physical-health/hypnic-headaches - August 12, 2022 – For two nights now I have not worked out. The goal is to be in a position that the attacks should happen. I drank two Cokes before bed. Around 70mg of caffeine. The second night I also felt as if I had something coming on, a migraine, sort of electrical buzz but no pain. No issues. I woke many times through the night and my dreams were absolutely insane, but no attacks.
I believe now that I have two things coalescing at once. Cyclic Variation of Heart Rate, where I wake from an apnea and my first respiration triggers an arrhythmia, fast and sometimes hard pounding heart rate. The second part is I believe my veins are constricted due to adenosine or otherwise related to a “Hypnic Headache”. That blood flow pushes through constricted veins causing a sever pain with each pulse and subsides as the arrhythmia ends. If I got up I would feel fine. I go back to sleep and the next time I awake it repeats for the same reasons.
Two nights is not enough but given the care I took to set up the scenario I am hopeful. That and everything fits. Caffeine pills should arrive today to replace the Cokes, which I no longer have a taste for. - August 18, 2022 – Caffeine continues to work. I have bradycardia many times at night, wake from REM often, but no throbbing and obviously no follow on pain. Its the pressure and the throbbing I care about. Neurologist is unwilling to research. Was trying a random drug for 3 months and would change after that but has no experience with this situation. He is also worried about the crossover responsibility of the heart in all of this. I doubt that personally. He doesn’t get paid for hard work. He gets paid to run a migraine meds mill and anything outside of his experience so far is apparently of no interest. This is my layman opinion. Nine months and a Coke would have cured me, well, of the symptoms, but those were the part that made it urgent. I will follow up to get a doctor’s diagnosis. For now, I appear to be good to chill a bit.
- August 19, 2022 – Last night I didn’t wake up midway and thus did not think to drink a partial Coke to add on to the caffeine. Made it through the night fine. 100mg pill at 730. Had been worrying about how long it would be good. Will for now stick to the pill.
- August 21, 2022 – Just a quick example of how I was manipulating my sleeping heart rate through exercise.
Preventing Bradycardia, heart beat below 60bpm
By exercising very hard during the day and usually in the evenings I would try to have my heart rate around 95bpm at 10pm at night when I fell asleep. This would keep my heart rate above 60bpm through all stages of sleep during the night. It was difficult to maintain but reduce opportunities for attacks. For me, no bradycardia meant no Cyclic Variation of Heart Rate and thus no fast heart beat leading to throbbing in the head with follow on pain. The lowest heart rate in this image is 61bpm at 5:40am.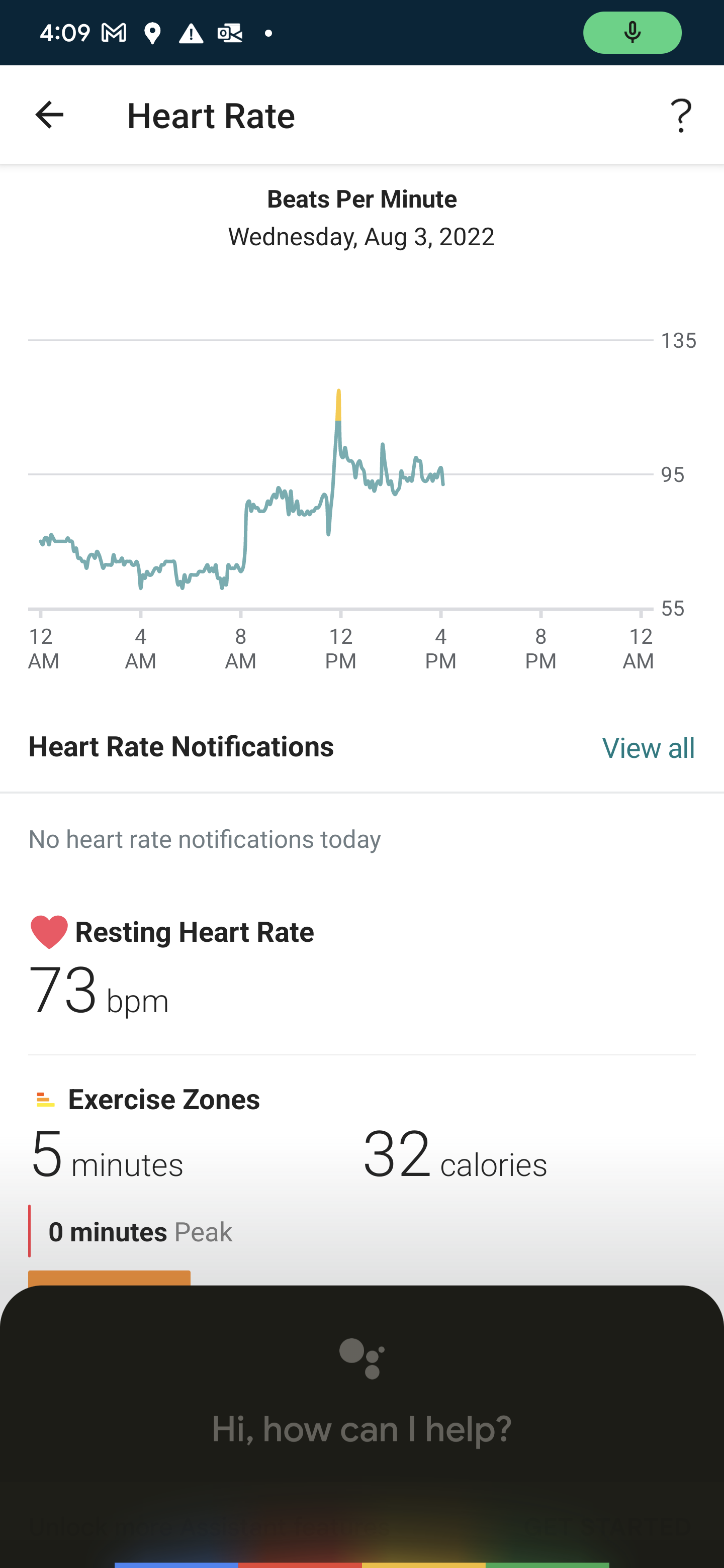
Intentionally enabling Bradycardia, heart beat below 60bpm
Once I wanted to test if caffeine worked, I decided to stop exercising for a week to make sure my body experienced bradycardia while sleeping. I needed to ensure the attacks could happen to test if caffeine stopped them. Anything below 60bpm is bradycardia, generally occurring between 4am and 6am. Years ago I usually had attacks around 6am. I say usually, they were not common but if they happened it was around 6am. Its only after going off caffeine entirely that I started to have them as early as 10pm but usually starting around 3am. This chart shows a low of 53bpm at 4:15am (55bpm at 6:20am) but you can see many periods below 60. 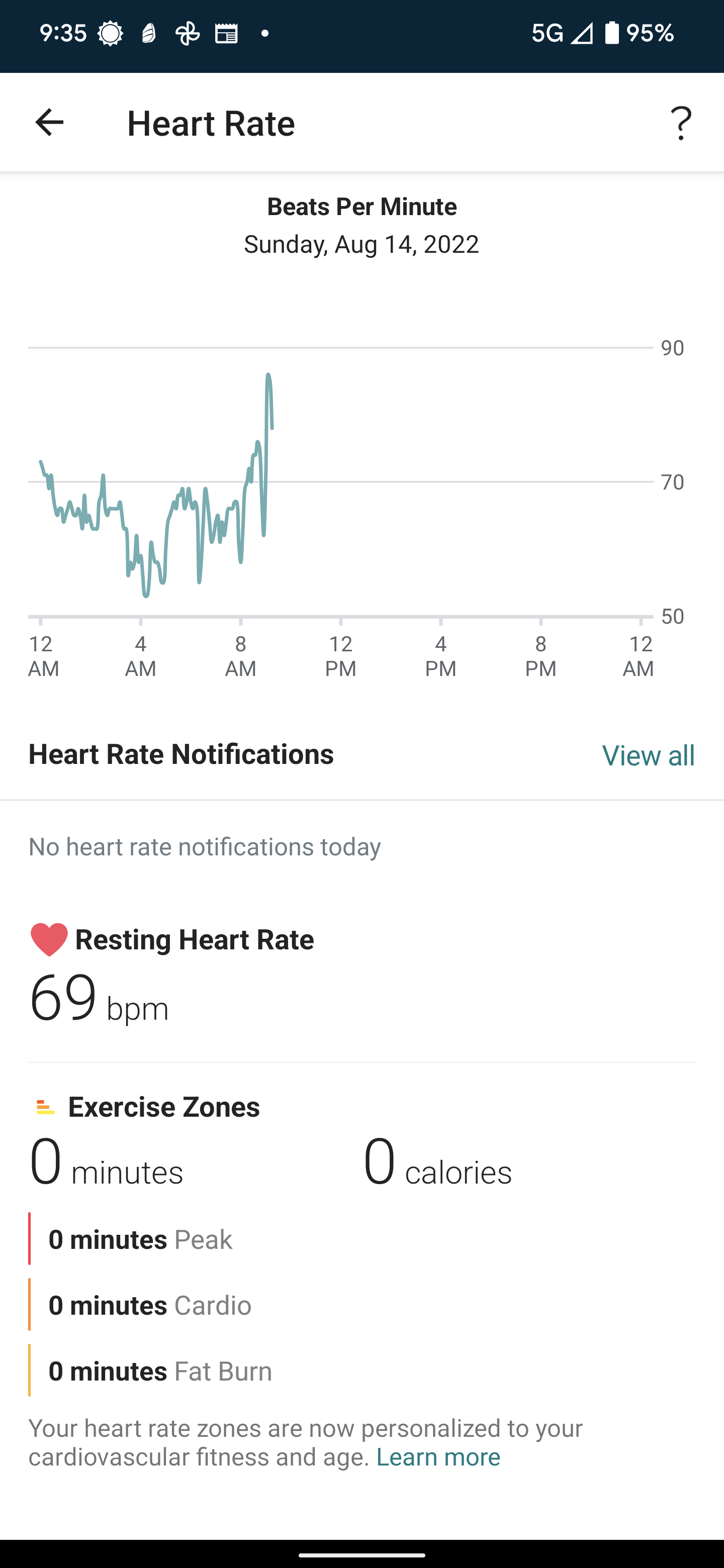
- Sept 6, 2022 – Woke from a vivid dream to find myself having a mild attack. Happened twice back to back. Wake, breathe, fast heart rate, attack, ends, rollover and breathe, fast heart rate, attack and end. 10s about each time. Milder than usual, not wincing escalating pain and a right temple vs neck. I didn’t drink caffeine during the day yesterday and the pill I took I took about an hour earlier than usual. So hoping it just mostly wore off over night. First arrhythmia I’ve detected since starting caffeine at bed time. Also first attack. Not horrible. Not wincing pain, maybe a 4 on the scale where the worst is an 8 to 9.
So from August 10 – Sept 5 no attacks while using Caffeine.
Went to rheumatologist today and he mentioned possibly going off of Hydroxychloroquine as it may cause arrhythmia. Will wait to go through sleep study and talk to doctor there. - Sept 7, 2022 – Woke up and paid attention to find an arrhythmia that lasted no more than 10s. So those still happen. No pain, no throbbing, no other indication but feeling the heartbeat faster. This was the first time I’ve noticed since I started caffeine. Probably because I don’t stay awake as long or wake enough anymore to notice.
- Sept 22, 2022 – Woke up during a particularly disturbing and vivid dream and found my heart racing and my head throbbing at base of neck more on right side and not feeling like the interior of my head so much. Not horrible, maybe a 2, but disconcerting. A constant pain instead of an increasingly severe pain. I had Coke several times during the day and took the caffeine pill around 9PM, late enough that it should have lasted. It was about 3:30AM. I got up a little later to let the dog out and there was the faintest throbbing still at the back right of the neck. Along the lines of a strained neck but clearly still the type of throbbing pain typical of these attacks. This was as I walked around. I debated drinking a Coke or not, do I want to see if it persists as I wake later or do I want to see if Coke will stop it? I’m drinking a Coke. Its 4:34AM.
I had one additional mild event and then things cleared up. My feeling is that I ate a late dinner of spaghetti and maybe that impacted absorption of caffeine from the pill. Pill should have lasted till 3:30AM but it may depend on exactly how much I need in my system, with a half-life of 6 hours.
Apparently caffeine is absorbed through mucus membranes and so when you have a full stomach that takes a bit to process the caffeine may be trapped in the food, taking time to touch the walls of the stomach, possibly some of it would not, and so food impacts absorption.
https://www.caffeineinformer.com/caffeine-absorption
https://www.caffeineinformer.com/caffeine-metabolism
https://www.caffeineinformer.com/the-half-life-of-caffeine
I was in bradycardia at 3:30AM. I also was at 6:30AM when I woke up during another dream and things were fine. Vivid dreams all night, which has not been typical lately. #NotAScientist - Oct 4, 2022 – I had a sleep study last night. To prepare, I skipped drinking caffeine during the day yesterday and also did not take the caffeine pill before bed last night. Study was done sans CPAP, so I was bound to have issues. At 6:08am and 7:17am I woke up, likely due to an apnea, felt a fast heart rate, and felt throbbing at the back of my head near the base of the skull, evenly on both sides with steady pain I would classify a 1 on a scale of 1-10. As in very mild pain and not 0, no pain. It was steady, did not escalate, and was never a 0. Most of my events start out with no pain and escalate to a 7 or an 8 (0,0,3,5,8,7,5) such that I feel the next one is going to be off the charts, but then it subsides with the arrhythmia and also as it spreads out like being soaked up by a sponge which sort of hurts more even as the intensity is lowering. According to FitBit, these two times and once at 4:16am were the only times I was in Bradycardia.
- Oct 10, 2022 – Found a conversation topic on Mayo. https://connect.mayoclinic.org/discussion/chronic-severe-nocturnal-hypnic-headaches/?pg=16#comment-759411
- Dec 3, 2022 – No issues, in fact I’ve grown tolerant of the caffeine, often sleeping 7 to 8 hours. Yes, some nights I stay up late but often I go to sleep quickly and then wake up after a couple of hours and I can go back to sleep fairly well. Not always, but so much better. I’ve recently tried lowering my dose with a tablet, taking it down to 75mg. While I have not had attacks, I did wake up with a headache yesterday. I’m having an issue with my gut. I don’t know if its related, isn’t timed particularly with starting to take the pills, but I wanted to see if I could lower my dose. I suspect I’ll stick with 100mg. At least until someone else tells me caffeine is causing me issues. I will add, I went to a sleep disorder doctor and he said I did exactly the right thing. That this is hard to diagnose, its rare and there is very little in the way of research, and having taken caffeine and it resolving things is sort of a confirmation that this is in fact Hypnic Headaches.
- June 9, 2024 – I continue to take 100mg caffeine pills nightly, with one recent exception. I went to Paris for a week. During that time I had Covid, jet lag, and typically walked 25000 steps a day. During the entire time I had no events. When I got back to the states and was catching up on sleep I had my first attack. I’m sure the bulk of the benefit came from walking so much. I did not monitor my heart rate at night, FitBit ran out of power two days in. Its also possible jetlag and Covid knocked my sleep patterns out of whack, certainly jetlag. But it was 7 days of sleeping without caffeine, which was great.
I can still generally go to sleep fine on caffeine. Its if I stay up at all after taking it that its an issue with not being able to go to sleep for hours. If I do go to sleep[ quickly, generally I wake up after about four hours and then I’m up for another one to two. It can sometimes be very annoying and tiring.
